Pulmonary fibrosis treatment is a multifaceted approach that encompasses a range of therapies, from medications to surgical interventions. Understanding the nuances of these treatments is crucial for patients seeking to improve their quality of life and overall prognosis.
As we delve into the complexities of pulmonary fibrosis treatment, we will explore the various options available, their mechanisms of action, and their potential benefits and risks. By empowering patients with knowledge, we aim to foster informed decision-making and ultimately improve outcomes.
Definition and Overview: Pulmonary Fibrosis Treatment
Pulmonary fibrosis is a chronic and progressive lung disease characterized by the scarring and thickening of lung tissue. This scarring makes it difficult for the lungs to function properly, leading to shortness of breath, coughing, and fatigue.Pulmonary fibrosis can be caused by a variety of factors, including:
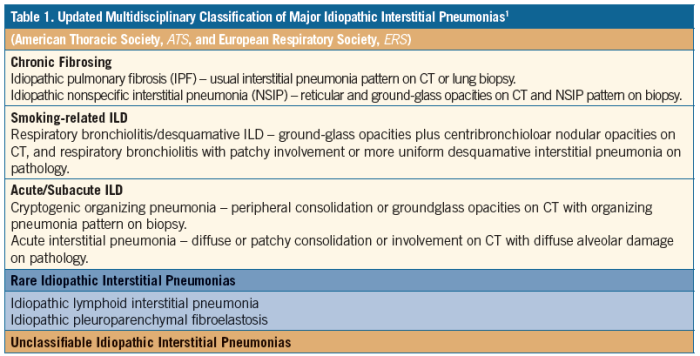
- Idiopathic pulmonary fibrosis (IPF): The most common type of pulmonary fibrosis, with no known cause.
- Secondary pulmonary fibrosis: Caused by another underlying condition, such as autoimmune diseases, infections, or exposure to toxins.
Pulmonary fibrosis is a serious disease that can lead to disability and death. It is estimated that approximately 200,000 people in the United States have pulmonary fibrosis, and the incidence is increasing.
Symptoms and Diagnosis
Pulmonary fibrosis often presents with a gradual onset of symptoms that can vary depending on the underlying cause and the severity of the condition. Common symptoms include:
- Shortness of breath, especially during exertion
- Dry cough that may persist for weeks or months
- Fatigue and weakness
- Chest pain or discomfort
- Wheezing or crackling sounds in the lungs
- Loss of appetite and weight loss
- Clubbing of the fingers or toes (in advanced cases)
Diagnostic Tests
Confirming a diagnosis of pulmonary fibrosis involves a combination of tests, including:
- Imaging techniques:
- Chest X-ray: Provides an initial view of the lungs and may show scarring or other abnormalities.
- High-resolution computed tomography (HRCT): A specialized imaging technique that produces detailed images of the lungs, allowing for better visualization of fibrosis.
- Biopsies:
- Lung biopsy: A procedure where a small sample of lung tissue is removed and examined under a microscope to confirm the presence and type of fibrosis.
- Lung function tests:
- Spirometry: Measures the volume and flow of air in the lungs, helping assess the severity of airflow limitation.
- Lung diffusion capacity test: Evaluates the lungs’ ability to transfer oxygen into the bloodstream.
Treatment Options
Pulmonary fibrosis, a progressive and irreversible lung disease, poses a significant challenge to patients and healthcare professionals alike. While there is no known cure, various treatment options are available to alleviate symptoms, slow disease progression, and improve quality of life.
These options range from medications and oxygen therapy to surgical interventions, each tailored to the individual needs and characteristics of the patient.
The choice of treatment depends on several factors, including the type and severity of pulmonary fibrosis, the patient’s overall health, and their preferences. A personalized treatment plan, developed in consultation with a pulmonologist or other healthcare professional, is essential to optimize outcomes and minimize potential side effects.
Medications
Medications play a crucial role in managing pulmonary fibrosis, primarily by reducing inflammation and slowing the progression of scarring in the lungs. Several types of medications are commonly used, including:
- Anti-inflammatory drugs:These medications, such as corticosteroids and azathioprine, help to reduce inflammation in the lungs, which can slow the progression of fibrosis.
- Anti-fibrotic drugs:These newer medications, such as pirfenidone and nintedanib, have been specifically developed to target the underlying mechanisms of fibrosis and have been shown to slow the decline in lung function.
- Immunosuppressants:These medications, such as cyclophosphamide and mycophenolate mofetil, are used to suppress the immune system, which can help to reduce inflammation and slow the progression of fibrosis.
It’s important to note that medications for pulmonary fibrosis can have side effects, and the choice of medication will depend on the individual patient’s needs and tolerance.
Oxygen Therapy
Oxygen therapy involves delivering supplemental oxygen to the lungs to improve oxygen levels in the blood. This can be done through various methods, including nasal cannulas, oxygen masks, or portable oxygen concentrators. Oxygen therapy can help to relieve shortness of breath, improve exercise tolerance, and enhance overall quality of life.
Surgical Interventions
In some cases, surgical interventions may be considered to treat pulmonary fibrosis. These interventions include:
- Lung transplantation:This is a major surgery that involves replacing the damaged lungs with healthy lungs from a donor. Lung transplantation is a complex procedure with significant risks, but it can offer a significant improvement in quality of life and survival for patients with severe pulmonary fibrosis.
- Lung volume reduction surgery (LVRS):This surgery involves removing a portion of the damaged lung tissue to improve lung function and reduce shortness of breath. LVRS is typically performed on patients with advanced pulmonary fibrosis who are not eligible for lung transplantation.
Surgical interventions for pulmonary fibrosis are typically reserved for patients with severe disease who have not responded to other treatment options. The decision to undergo surgery should be made in consultation with a pulmonologist and other healthcare professionals.
Medications
Medications play a crucial role in managing pulmonary fibrosis, aiming to slow the progression of the disease and improve lung function. Various types of medications are used, each targeting different aspects of the disease process.
The table below provides a comparison of different medication classes commonly used in pulmonary fibrosis treatment:
| Medication Class | Mechanism of Action | Examples |
|---|---|---|
| Antifibrotic Drugs | Inhibit the formation and accumulation of scar tissue in the lungs | Pirfenidone, Nintedanib |
| Immunosuppressants | Suppress the immune system to reduce inflammation and fibrosis | Azathioprine, Mycophenolate mofetil |
| Corticosteroids | Reduce inflammation in the lungs | Prednisone, Budesonide |
Antifibrotic Drugs, Pulmonary fibrosis treatment
Antifibrotic drugs are a newer class of medications specifically developed to treat pulmonary fibrosis. They work by inhibiting the production of collagen and other proteins involved in scar tissue formation.
Examples of antifibrotic drugs include:
- Pirfenidone
- Nintedanib
Studies have shown that antifibrotic drugs can slow the decline in lung function and improve symptoms in patients with pulmonary fibrosis.
Immunosuppressants
Immunosuppressants are medications that suppress the immune system. They are used in pulmonary fibrosis to reduce inflammation and fibrosis.
Examples of immunosuppressants include:
- Azathioprine
- Mycophenolate mofetil
Immunosuppressants can be effective in reducing inflammation and fibrosis in pulmonary fibrosis, but they can also increase the risk of infections.
Corticosteroids
Corticosteroids are medications that reduce inflammation. They are often used in pulmonary fibrosis to reduce inflammation in the lungs.
Examples of corticosteroids include:
- Prednisone
- Budesonide
Corticosteroids can be effective in reducing inflammation in pulmonary fibrosis, but they can also have side effects such as weight gain, fluid retention, and increased risk of infections.
Oxygen Therapy
Oxygen therapy is a crucial treatment for pulmonary fibrosis, aimed at increasing oxygen levels in the blood and reducing the symptoms associated with the condition. It involves delivering supplemental oxygen to the lungs through various methods, including nasal cannula, oxygen concentrator, and mechanical ventilation.
Nasal Cannula
A nasal cannula is a thin, flexible tube with two prongs that fit into the nostrils. It delivers a continuous flow of oxygen directly into the nasal passages. Nasal cannula is commonly used for mild to moderate cases of pulmonary fibrosis and is relatively comfortable and easy to use.
Oxygen Concentrator
An oxygen concentrator is a device that separates oxygen from the surrounding air and delivers it at a higher concentration. It is typically used for patients with more severe pulmonary fibrosis who require higher levels of oxygen support. Oxygen concentrators are larger than nasal cannulas and require an electrical outlet to operate.
Mechanical Ventilation
Mechanical ventilation is used for patients with severe respiratory failure who are unable to breathe adequately on their own. It involves using a machine to assist or control breathing. Mechanical ventilation can be invasive, requiring a tube to be inserted into the trachea, or non-invasive, using a mask or nasal prongs.
Benefits of Oxygen Therapy
Oxygen therapy provides several benefits for patients with pulmonary fibrosis:
- Increases oxygen levels in the blood, improving overall oxygenation and reducing shortness of breath.
- Reduces symptoms such as fatigue, confusion, and headaches.
- Improves sleep quality by reducing nighttime oxygen desaturation.
- Slows the progression of pulmonary fibrosis and improves overall quality of life.
Indications and Contraindications
Oxygen therapy is indicated for patients with pulmonary fibrosis who have low blood oxygen levels or experience symptoms related to oxygen deprivation. It is contraindicated in patients with chronic obstructive pulmonary disease (COPD) or other conditions where high oxygen levels can suppress the respiratory drive.
Surgical Interventions
Surgical interventions play a crucial role in treating advanced cases of pulmonary fibrosis when other therapies prove ineffective. These procedures aim to alleviate symptoms, improve lung function, and potentially extend life expectancy.
Lung Transplantation
Lung transplantation involves replacing the diseased lungs with healthy donor lungs. It is considered the most effective surgical option for end-stage pulmonary fibrosis patients who meet strict selection criteria, including being relatively young, having a good overall health status, and being able to tolerate immunosuppressive medications.
Lung transplantation offers significant potential benefits, including improved lung function, reduced symptoms, and increased survival rates. However, it also carries significant risks, such as the potential for rejection, infection, and complications from immunosuppressant drugs.
Bullectomy
Bullectomy is a surgical procedure that involves removing large air-filled sacs (bullae) from the lungs. These bullae can compress healthy lung tissue, leading to shortness of breath and other respiratory problems.
Bullectomy is typically performed on patients with advanced pulmonary fibrosis who have large, symptomatic bullae. It can improve lung function and reduce symptoms, but it does not cure the underlying disease.
Complementary Therapies
Complementary therapies, while not a cure for pulmonary fibrosis, may offer symptom relief and improve quality of life. These therapies include pulmonary rehabilitation, acupuncture, and yoga.
- Pulmonary Rehabilitationinvolves exercise training, education, and support to help patients manage their symptoms and improve their overall well-being.
- Acupunctureis a traditional Chinese medicine technique that involves inserting thin needles into specific points on the body to stimulate the release of endorphins and reduce inflammation.
- Yogacombines physical poses, breathing exercises, and meditation to promote relaxation, reduce stress, and improve lung function.
The potential benefits of these therapies include:
- Reduced shortness of breath and fatigue
- Improved exercise capacity
- Enhanced quality of life
However, it is important to note that these therapies are not a substitute for medical treatment and should be used in conjunction with prescribed medications and therapies. Patient Education and SupportPatient education and support play a crucial role in improving outcomes in pulmonary fibrosis.
Patients who are well-informed about their condition and have access to support groups and resources are better able to manage their symptoms and cope with the challenges of the disease. Support groups provide a sense of community, emotional support, and practical advice from others who understand the challenges of living with pulmonary fibrosis.
Prognosis and Outlook
The prognosis for pulmonary fibrosis varies widely depending on the type and severity of the disease. In general, the earlier the diagnosis and treatment are initiated, the better the outcomes tend to be.
Factors that can influence the prognosis of pulmonary fibrosis include:
- Age and overall health
- Type and severity of pulmonary fibrosis
- Response to treatment
- Presence of other medical conditions
Impact of Early Diagnosis and Treatment
Early diagnosis and treatment of pulmonary fibrosis can significantly improve the prognosis. Early intervention can help slow the progression of the disease and prevent further lung damage.
If you have any symptoms of pulmonary fibrosis, it is important to see your doctor promptly for evaluation and diagnosis.
Current Research and Emerging Therapies
There is currently no cure for pulmonary fibrosis, but there are a number of treatments that can help slow the progression of the disease and improve symptoms. Researchers are also working on developing new and more effective treatments for pulmonary fibrosis.
Some of the most promising emerging therapies for pulmonary fibrosis include:
- Anti-fibrotic medications
- Stem cell therapy
- Gene therapy
Outcome Summary
Pulmonary fibrosis treatment is an evolving field, with ongoing research paving the way for new and innovative therapies. By staying abreast of these advancements and tailoring treatment plans to individual patient needs, we can optimize outcomes and provide hope to those affected by this challenging condition.
Top FAQs
What are the common symptoms of pulmonary fibrosis?
Shortness of breath, dry cough, fatigue, and crackling sounds in the lungs are common symptoms.
How is pulmonary fibrosis diagnosed?
Diagnosis involves a combination of physical examination, imaging tests (such as chest X-rays and CT scans), and lung function tests.
What is the prognosis for pulmonary fibrosis?
The prognosis varies depending on the type and severity of the condition, but early diagnosis and treatment can improve outcomes.